Medication was a serious subject
I found no humor in caregiving until I pulled back the curtain and saw it for what it was. It was seriously hard and at times seriously funny. Language is also a funny thing. How did the word “seriously” come to mean “very”? This language confused my French students who were learning English, like how something can be “pretty” ugly. I hope reading about our steps and missteps is helpful as you navigate your way through the maze of medication management. This is for general information only; please contact your health care team for guidance on your particular situation.
God is a comedian playing to an audience too afraid to laugh. — Voltaire
Medication was a serious subject and as a new caregiver, managing it was one of the most daunting responsibilities I faced. I was certain that I could make a mistake that might result in Dad’s death. This was not a completely unfounded fear. According to the Food and Drug Administration, 1.3 million people are injured by medication mismanagement. 140,000 older adults die each year from taking prescription medication improperly. 28% of senior hospitalizations in the US are caused by medication related problems. Here are some tips from AARP about how to avoid medication errors.
Getting organized
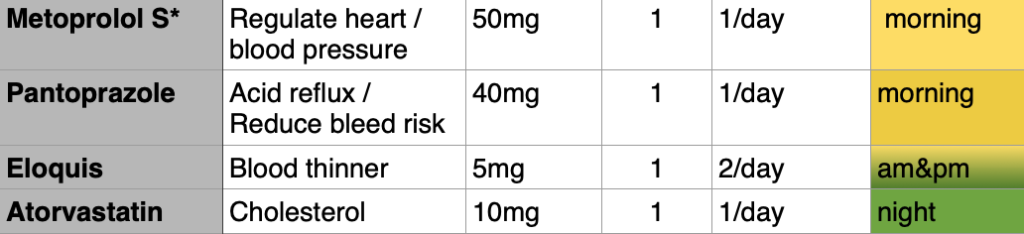
Dad had been sorting and taking the pills on his own prior to the stroke. Post stroke, I made a list of his meds and color coded them based on morning, evening and a blend of the two colors for the pills that he took both in the am and pm. In addition to the medication; the purpose, dosage, quantity and frequency were listed. All that was missing was the phonetic pronunciation. I reveled in the reaction of the healthcare professionals when I handed them my project. I was organized, competent, color coded. The lesson, yet to learn, was that that was the easy part of managing meds. It was smoke and mirrors, the illusion of control. My color coding gave me confidence and at the end of the day, that was the real value.
I also started a binder of medical details. I included a spreadsheet of physicians and visits. Notes of the discussion during the visits were kept here. Most often this was a written record, but sometimes with the doctor’s permission, I used an app called Abridge. This was helpful to have as a reference when there were conflicts or confusion about what was said by the doctor. The notebook was a great place to keep track of symptoms and changes in Dad’s behavior.
Sifting, sorting, separating
Post rehab, Dad accepted and appreciated that I kept his meds straight considering that prescriptions had changed and his mind was still fuzzy. When he was ready to return to his sorting role, he wasn’t just insistent that he take over, but adamant. Medication for both of us represented independence. I dreaded the day that he could no longer manage his medicines. If he could no longer take them from a pill container, what would that mean for our collective freedom?
Quantity vs Quality
Dad took nine prescription pills and five doctor recommended supplements. This was a bit more than the average senior living at home, but closer to the average taken by a senior in a nursing home. Each visit to the doctor, I asked that we re-evaluate the mix of meds to determine if we could eliminate any of them. The doctor was reluctant. Dad was 98. The melange was working. But was it? There is little guidance for when to stop a medication. Not only are some medications unnecessary in older adults, they may be unsafe. Dad was in favor of reducing the quantity of pills he took, but he was not a fan of the process. Tapering and trial and error needed to be managed by a physician and the results closely monitored. We recently eliminated one of Dad’s medications, modified another and may start the process to reduce one more. The key to safety has been to have the conversation and coordinate with Dad’s physician.
As Dr Gerado Moreno says in the US News article, How to Safely Reduce the Medications You Take, “’I think a caution for patients trying to reduce the number of prescribed medications is that they should talk to their doctor first’ before making any changes, he says. Some medications, for example, can’t be safely stopped cold turkey. ‘But also [patients should] ask their doctor to make sure that they are taking indicated, evidence-based medications that are shown to improve their long-term health outcomes.’”
Side effects
Dad frequently reported feeling wobbly and tired. This was understandable considering his age, but these were also common side effects of several of the pills he took. In addition, he out-aged the medication that he used for sleeping and this was brought to our attention by the insurance company pharmacist. I talked over Dad’s medication once a month with one of these patient Clinical Pharmacists and I always learned something of value. Initially, I considered it a way for the insurance company to make sure Dad was as profitable as possible. After a few calls, I began to appreciate their role and respected the information they shared that often led to a productive conversation with the PCP, a tweak in a prescription or two and several times saved us money.
Dad’s PCP was very collaborative. Even so, I knew it was not easy to have yet one more outside interest suggest how he function in his role. I respected his openness to discuss whatever new question or concern arose from the conversation I had had with the insurance company. Since he also got a copy of the conversation summary letter, he was most often ready with options. Side effects of any drug may be researched on the US National Library of Medicine website. Drugs.com offers the opportunity to check for medication interactions as well as other important information including how drug interactions occur and what other factors may cause interactions.
Transfer of responsibility
Low vision and poor dexterity eventually made sorting too difficult for Dad. Joe and I took trips that sometimes lasted weeks, so I sorted Dad’s medicines into a 31 day pill container. It was a project, but when done, Dad was able to manage the process. Joe and I were able to take mini trips with the addition of aides who helped out 9 hours a week. Dad decided that he could make improvements to the system. One day, I noticed that the boxes were unordered, days mixed up and half were flipped upside down from day to night, pills were also out of place in half of the 31 boxes. It looked like it took a lot of effort to reorder and reimagine this new scheme.
Today I got my happy pills and my ticked off pills mixed up. I took one of each so now I’m ticked off but I’m happy about it. – Unknown
Dad was not interested in a conversation about what had happened or why. The system was no longer working because Dad was no longer happy with it. He requested to try sorting on his own again. I left him to his work. Pills were doubled up on some days and missing from others. I would do the sorting, but the 30 day container was no longer an option.
Finding the right pharmacy
I researched the national and local pharmacies that offered pill sorting. Then, I called them to better understand the difference in services and the benefits of each option. The final solution was a local pharmacy that delivered a month’s sorted pills at a time. If a change was needed mid-month, they picked up, re-sorted and re-delivered. Dad reluctantly accepted and successfully converted to the new system. After a year of smooth operating, the insurance company no longer worked with this pharmacy. I selected a pharmacy recommended by the insurance company. Transitioning was an ordeal. After a few months, I determined that the relationship was not workable. The service was poor, and the customer service worse.
With great fortune, the former pharmacy called; their sister pharmacy in the next county was still working with Blue Cross, so we were back in business with a local pharmacy that offered great service. This pharmacy group supplied many of the area nursing homes with medicines. We were just a bit of add-on business, but we were treated with respect and phenomenal service. We used a drug store pharmacy, that was open on weekends, to supplement the less regular needs which included:
- Two medications that were taken as needed
- Eye drops that treated macular degeneration and glaucoma symptoms
- Temporary medication needed to resolve short term issues such as a UTI or pneumonia
The pharmacist as a resource
Drug store pharmacists were a fantastic source of information and guidance. One in particular, shared a useful tip. She said that Saturday and Sunday, late afternoon, was a very slow pharmacy period and the perfect time to get some extra help, often with undivided attention. The pharmacist was the perfect resource when I was unsure how an over the counter medicine might interact with Dad’s prescriptions.
Joan Baird is director of pharmacy practice with the American Society of Consultant Pharmacists. She cautions, “Because older adults metabolize (break down) medications more slowly, drugs can hang out in their body longer, Baird says – and a drug that might make a younger person feel slightly tired the next day could leave a senior lightheaded when they get out of bed.” Benadryl was one of the many OTC options that we needed to avoid. The ingredient, diphenhydramine, caused trouble and was hidden in plain sight in many other OTC medications.
Couldn’t we please schedule UTI’s
Dad’s UTI’s typically showed up in full symptom form on Friday’s at 5pm. It was uncanny. His mode of operation was to not tell me until it had been several days that he couldn’t make it to the bathroom in time. Once, I found out when my coffee thermos top went missing overnight from the dish drainer. I asked Dad if he had seen it. Yes, he had. It was on a bottle that he had put beside his bed to pee in because he wasn’t making it to the toilet. This discovery happened early on a Saturday morning. I ordered another lid from Amazon, went for a run and told Dad we would go to the urgent care clinic when I returned.
Grim care, moroseness, and anxiety—all this rust of life ought to be scoured off by the oil of mirth. Mirth is God’s medicine. — Henry Ward Beecher
It was not unusual for Dad to not share something that would, without question, require medical attention. It had happened so many times in the past that asking Dad the, “Why didn’t you mention this sooner”, question and requesting that he let me know of a problem before it was urgent, was more like a recording than a conversation. His response was predictable, “I don’t know why I didn’t tell you sooner.” I understood his hope that it would just go away, get better or “maybe I imagined it”. A more proactive approach would have been for me to put it on a checklist to ask weekly, “How’s the peeing going.” I realized that I was resisting the routine that would reduce the unpredictability.
Minor mishaps made great humor
We had minor mishaps with the pre-packed pill system. Occasionally, we found pills on the floor. We brought it to Dad’s attention without making it a deal, just to reinforce that he be careful. His response was often, “How the heck did that get there?”, said with absolute incredulousness. We learned to toss the fallen pill immediately into the trash. Otherwise, he would ask to see it, take it for a closer look and put it into his mouth. The evidence was gone, so it never happened.
From there to here, from here to there, funny things are everywhere. — Dr. Seuss
One morning, our aide put two pills on the coffee table that she found on the floor. While she went to identify them, he popped them into his mouth. They were melatonin for sleeping. That changed the plan for the day. A neighbor did the same, found a pill on the floor and put it on the table. He swallowed it before she could say, “Noooo!!”. The look on her face was priceless. This did not happen often, but over the course of years. The first time, I overreacted and madly tried to figure out what he had taken and determine if I needed to call the CDC. Similarly amusing was Dad’s response when we asked what happened to a morning or evenings pills taken in error. He sincerely did not know where they could have possibly gone and was genuinely as surprised as we were that they were missing.
Next level plan
The only thing consistent in caregiving is that things will change. Two changes happened almost simultaneously to upset our pharmaceutical flow. The first was that Hospice began to provide three of Dad’s medications and they were delivered from their pharmacy. Since his medications began coming from two sources, I was back in the sorting business. We returned to weekly containers, white for daytime, green for evening. This worked for a while and then the mistakes became too frequent. He forgot that he took his morning meds and took them twice. Then, he took his nighttime meds in the morning. That was a quiet day, other than the snoring.
Tighter controls
We considered an automatic dispenser, but never quite bought into that solution. Instead, we purchased sauce or condiment cups. After more significant mistakes were made over the span of several weeks, we had the conversation with Dad. It didn’t go well. He got spitting angry at the suggestion that morning and evening, we set out his meds in a cup. He suggested another solution. I was doubtful, but agreed. He put the nighttime container next to his bed and left the daytime container on the coffee table. Unfortunately, that went off the rails within a week. Twice, he took his nighttime meds twice and once did not take his daytime meds until we checked it later in the day.
Even though we had been ready with the next level medicine plan, we had been resistant to implement it for a few reasons. We knew that Dad would not be easily persuaded to make this change and we knew it meant that we would be even further travel-restricted. COVID-19 made the last fear a reality sooner than the status of medication management. It was time to take the big step.
Tough transition
We were not in a happy place for weeks. Dad said he wouldn’t take his pills if he couldn’t have it his way. I said, “No problem.” We would set the meds out morning and evening, he could take them whenever he wanted or not at all if that’s what he chose. Joe was the better of us to take the meds to Dad, but Joe was trying to stay on the calm side of this conflict, so he tried to put them on Dad’s coffee table when Dad wasn’t there or was sleeping. This resulted in a missed night of night meds and hell to pay the next morning.
Dad said some hurtful things, scrunched his face up and directed at me, “What’s wrong with you? You’re enjoying this…” He asked me if I was trying to get revenge for something he did during my childhood. He had already forgotten the mistakes he made when we separated the daytime and nighttime meds and really thought we were being unreasonable and spiteful. His words could have been hurtful, but they washed over me, not penetrating my heart. This part we just had to endure, wait it out, stay calm, stand firm. David Solie offers crucial advice to help everyone navigate through the toughest decisions in his book, How to Say it to Seniors.
Curiosity
Curiosity helped me keep perspective. How much of what he said would he remember? Might he apologize? Would we repeat the confrontation later that day, then again the next? Would he accept the change and not discuss it again? All of these were possible. I held my phone and recorded as we were talking. I was talking, he was yelling and putting his hand up when I started to speak. My hope was to assess if I could have handled the situation better. I could have. As I was watching, I saw the desperation and inner turmoil. The pain.
I thought back to a story Dad shared occasionally and then later read in his journal. He lost his first child, a boy, as an infant. He had to give last rights when the priest couldn’t get there in time. It was the hardest thing he had ever done, has ever done. He taught high school and on the day he returned to class, the principal had told the students that my parents had lost their child. There was silence in the classroom when he entered. To break the ice, Dad told a joke, something about an automatic washing machine not being automatic because he still had to load and unload it. It worked. The kids laughed. He started teaching. This demonstrated his true character.
Respect
It was important for me to remember that Dad was an accumulation of all of his experiences, not this one moment of resistance, anger and emotion. Joe, Dad, and I all played a part in getting us through this adjustment as smoothly (or not) as possible. Dad’s participation was framed by the losses he had already experienced as he worked his way to 98. He had given up tennis, golf, travel, driving. Over the years, he had lost those closest to him, his wife, his friends, classmates and shipmates. His eyesight and hearing were severely diminished. We brought him his meals and delivered supplies from his lists. He remarked once that Amazon must be quite a store. He appreciated it, but it was not how he preferred to exist, relying on someone else, making the list and then handing it over.
Each of these losses represented a chip at his dignity and this latest one was a chunk. His disbelief wavered between two inconceivable truths.
- The knowledge that we believed that he was not capable of taking medicines from a pill container.
- The realization that he was not capable of taking medicines from a pill container.
Either way, the anger, fear and resentment that he felt were overwhelming. Those emotions matched the anger, fear and resentment that I was feeling. The difference was that it was my responsibility to get us through this with love and hopefully be able to look back with some laughter.
Navigating the Caregiver River: A Journey to Sustainable Caregiving is available on Amazon. Also, check out the Self-Caregiving Strategies Podcast.
Schedule Theresa Wilbanks to speak on caregiving and empower the caregivers in your workplace or community with the 12 Sustainable Caregiving Strategies.
Advice offered is for general information only; please contact your healthcare team, legal or financial advisors to guide your particular situation.

